Incident Management
Policy Scope
Postural Innovations takes the safety and wellbeing of the people it supports very seriously and as such incidents involving both the people we support, and our staff are treated as a high priority.
This policy is designed to:
provide governance that clearly outlines the responsibilities of personnel in incident management;
provide a system that facilitates the identification, reporting, reviewing, monitoring and evaluation of all incidents in a timely and effective manner;
ensure those involved in, or affected by, incidents receive appropriate assistance and support;
ensure organisational learning from incidents, including near-miss events and system failures, to mitigate future risk;
increase awareness of reporting requirements and related legislation.
Policy Principles
The principles of the policy are:
Obligation to Act – There are clearly defined roles and responsibilities in the incident management process that are acknowledged and understood by the key stakeholders.
Just Culture – Incidents are reported and acknowledged without fear of blame or retribution and individuals are treated fairly in an open and honest manner.
Prioritisation of Action – Actions to assist in the investigation (review) of incidents are prioritised by Postural Innovations in order to facilitate timely and effective reviews of high impact incidents.
Emphasis on Learning – The policy is focused towards learning from incidents in order to create a patient safety learning culture across Postural Innovations services.
Legislation, regulations and standards relevant to this policy and procedure include:
Responsibilities
Directors
Postural Innovations Directors will:
ensure the organisation has systems in place to report, investigate and monitor actions necessary to reduce the likelihood of incidents recurring;
ensure sufficient mechanisms are in place to enable the effective reporting, recording, investigation and implementation of recommendations as a result of an incident;
ensure staff are encouraged (and supported) to report incidents and near-miss events as a proactive preventative measure;
ensure recommendations derived from incident investigations are appropriately addressed and their effectiveness is evaluated;
ensure the principles of open disclosure are observed when interacting with patients and their families or carers when an incident occurs and that these principles guide the overall management of the incident;
ensure all sentinel events and clinical Incident Severity Rating Level 1 incidents where the organisation has identified system or process issues directly contributed to the incident outcome, are reported to the NDIS commission;
encourage and support staff through training of incident management processes (including open disclosure) and should encourage an environment where incident notification and active management of incidents (and near misses) is fostered.
Consultants
Postural Innovations Consultants will:
manage incidents and ensure the learning gained and recommendations from investigation and review processes are fully implemented, monitored and their effectiveness evaluated;
ensure timely notification and investigation of incidents in accordance with Postural Innovations Risk and Hazard Management policy and Postural Innovations Adverse Incident Policy;
ensure feedback on recommendations of incident reviews are provided to those who reported the incident and those involved in the management or investigation of the incident.
Staff
All Postural Innovations staff are responsible for:
notifying a Director of an incident at the time of the event;
reporting incidents in using the Incident and Hazard Report Form;
participating in the investigation and review of incidents as required;
participating in the implementation of recommendations arising from investigation of incidents.
The Incident Management Process
There are (7) seven steps to effective incident management:
Identification
Notification
Prioritisation
Investigation
Classification
Analysis and Action
Feedback
1. Identification
It is important for all staff to recognise when an incident has occurred. An incident is defined as an act, omission, event or circumstance which could have, or did, lead to unintended and/or unnecessary harm.
The incidents which must be recorded and managed are:
incidents which have, or could have, caused harm to a person with disability receiving supports or services; and
acts by a person with disability that happen in connection with the provision of supports or services and that have caused serious harm, or a risk of serious harm, to another person; and
reportable incidents that are alleged to have occurred in connection with the provision of supports or services. Refer to Risk and Hazard Management Policy and Abuse and Neglect Policy.
Identification of an incident will only be achieved in a culture and environment which allows this to happen without fear of retribution, and where incidents (and the reporting of incidents) are an acceptable part of healthcare delivery. Postural Innovations aims to foster this culture. Identification of an incident is not only limited to what is observed but also includes where a person with a disability informs staff of an incident.
Following identification of an incident or near-miss there may need to be immediate action.
These actions may include:
providing immediate care to individuals involved in the incident (clients, staff or visitors) – refer to steps in Adverse Incident Policy and Procedure;
making the situation or scene safe to prevent immediate recurrence of the incident;
notify the director an incident has occurred;
removing malfunctioning equipment or supplies;
gathering basic information about a chain of evidence;
notifying police and security.
2. Notification
Staff are required to notify all incidents and near-miss events by filling out an Incident and Hazard Report Form located in SharePoint and sending this form to the Directors – Steve Woollard and Angela Rowe, for review. Refer to Adverse Incident Policy and Procedure.
All clinical incidents must be documented in SharePoint by the consultant/therapist. Care must be taken to ensure only clinically relevant and factual information is included in this note.
Reporting an incident must occur as soon as practicable (within 2 hours for Severe or Major incidents) and preferably is to occur by the end of the notifier’s workday.
Postural Innovations, as a registered NDIS provider, is only required to notify the Commission of reportable incidents which have occurred, or are alleged to have occurred, if those incidents happened in connection with the provision of supports or services provided by us. Reportable incidents under the NDIS Commission are:
the death of a person with disability; or
serious injury of a person with disability; or
abuse or neglect of a person with disability; or
unlawful sexual or physical contact with, or assault of, a person with disability; or
sexual misconduct committed against, or in the presence of, a person with disability, including grooming of the person for sexual activity; or
the use of a restrictive practice in relation to a person with disability, other than where the use is in accordance with an authorisation (however described) of a State or Territory in relation to the person.
Incidents are to be reported to the following people:
Steve Woollard and Angela Rowe (Directors of Postural Innovations) of all incidents – who will then notify the NDIS Commissioner of reportable incidents;
Family members, carers and guardians (as per consent form or legal contact recorded on SharePoint);
Client’s support coordinator;
Police – as outlined in the Abuse and Neglect Policy;
Emergency services – as outlined in the Adverse incident Policy.
It is important for Notifiers to give as much information as possible to assist further review and management of the incident and allow optimal classification of incidents and comparison of data. The Incident Report should contain factual information, not individual assumptions of what occurred.
The patient and their family or carer can notify Postural Innovations of an incident through the online Feedback Form or via the paper form contained in the Postural Innovations Welcome Pack.
Incident notification – Director’s responsibility
The Directors are required to review the incident notification and assist staff in completing the Postural Innovations Incident and Hazard Form. After receiving the form, the Directors will then derive the Incident Severity Rating (ISR) according to the actual incident outcome or near-miss based on the answer to three questions:
degree of impact;
level of care;
treatment required.
Notification to patient (open disclosure)
All clinical ISR 1 and 2 events are to be managed by the open disclosure process. The initial disclosure to the client or their support person must occur within 24 hours of the incident, or as soon as is practicable, by the staff responsible for the care of the patient or an appointed delegate.
When a clinical incident occurs to a client, an integral component of the notification process is to acknowledge the occurrence of the incident to the client and their support person, as appropriate, inform them of the type of investigation that will be undertaken, give an opportunity for the affected patient to relate their experience and inform them of the steps taken to manage the event and prevent its recurrence. An apology for the incident suffered is given at this stage.
3. Prioritisation
The purpose of prioritisation is to ensure a standardised, objective measure of severity is allocated to each incident or near-miss. This enables an appropriate level of investigation to be conducted.
The ISR is used to prioritise all notifications. The ISR was developed based on the World Health Organization (WHO) Incident Classification for Patient Safety (ICPS) Conceptual Framework. Postural Innovations will derive the ISR from the responses to the three questions relating to:
degree of impact;
level of care;
treatment required.
The ISR rating guides the level of investigation and the need for additional notification.
ISR 1 – Severe/Death
ISR 2 – Major
ISR 3 – Moderate
ISR 4 – Minor (near-miss / no harm)
All ISR 1 incidents should be notified to a Director of Postural Innovations – Steve Woollard or Angela Rowe – through the incident report form and an email.
All clinical ISR 1 incidents where the organisation has identified system or process issues directly contributed to the incident outcome require a detailed and thorough investigation using the Root Cause Analysis (RCA) methodology. Clinical ISR 1 incidents not deemed to be related to Postural Innovations system or process issues should be reviewed with either in-depth case review or RCA methodology.
All ISR 1 and ISR 2 clinical incidents where the organisation has identified system or process issues directly contributed to the incident outcome are to be notified to the NDIS Commissioner.
4. Investigation
Investigation of the incident is an important component of any patient safety program. All incidents notified in the Postural Innovations Incident Reporting Log require an investigation or review process. Investigations conducted under this policy should not canvass issues of individual performance. Where a question of individual performance arises, this is to be managed via the organisation’s Performance Management System. During investigation, Postural Innovations will ensure people are afforded procedural fairness and all incidents, irrespective of their ISR rating, require a review to assess the level of investigation required.
The ISR rating guides the level of investigation. All health services should:
assign appropriate levels of responsibility for investigation and management of all incidents;
have policies and procedures in place to guide the investigation of incidents that reflect the principles of open disclosure;
have staff training programs in place for investigation of incidents;
have appropriately trained staff to support staff involved in incident investigations;
ensure feedback mechanisms are in place so that staff and clients are informed of outcomes related to incidents reported;
all ISR 1 clinical incidents where the organisation has identified system or process issues directly contributed to the incident outcome receive a detailed and thorough investigation using the RCA methodology;
all ISR 1 clinical incidents where the organisation has identified the contributing factors to the incident outcome relate directly to the patient’s illness or management phase of their chronic illness require an in-depth case review;
all ISR 2 incidents are investigated using the in-depth case review methodology or principles;
all ISR 3 and 4 incidents are reviewed as an aggregate (as a minimum) over a monthly period.
ISR 1 Incidents
All ISR 1 incidents will be reviewed by a Director of Postural Innovations to determine causation and opportunities for system improvement within 28 working days of the incident notification date.
On identification of an ISR 1 clinical incident, the Director is to review the incident to determine whether the outcome was directly related to system or process issues.
If this initial review signifies organisational processes contributed to the incident outcome, an RCA is to be undertaken to explore causation and identify contributing factors, and notifications are to be made following the steps in the Postural Innovations Adverse Incident Policy.
The summary report of the ISR 1 incident investigation should be presented to the team involved in the care of the patient. The outcomes should also be presented or made available to the relevant staff involved in the patient care to ensure staff are aware of the factors contributing to the incident and the action being taken to improve safety.
Recommendations stemming from the RCA report, where possible, should be linked to the Postural Innovations Risk Register to ensure continuity of the monitoring of both the evaluation and effectiveness of the recommended actions as a risk management strategy.
ISR 2 Incidents
All ISR 2 incidents will undergo a detailed investigation of the incident preferably utilizing the in-depth case review methodology template on SharePoint within 28 working days of the incident notification date.
Ongoing monitoring of trended aggregated incident data may also identify and prioritise issues requiring a quality or practice improvement project.
ISR 3 & 4 Incidents
The investigation of ISR 3 and 4 incidents will be undertaken by the director for review and processing within 60 working days of incident notification.
Monitoring of trended aggregate incident data may also identify and prioritise issues requiring a quality or practice improvement project.
Reports and analysis of aggregate ISR 3 and 4 incidents should be made known to the staff and persons affected by the incident to identify opportunities for change.
Consideration should be given to providing clients and their families/support network with the opportunity to contribute information about the clinical incident to assist with the investigation process and the development of patient-centred recommendations.
5. Classification
This is the process of capturing relevant information from a range of perspectives about an incident to ensure the complete nature of the incident, including causative, contributory and preventative factors, are documented and understood.
Classification is undertaken by the Directors. It is important all fields in the Postural Innovations Incident and Hazard Report Form are completed for each incident. This will assist in the classification as well as the development of strategies based on trended data to understand cumulative risk and to minimise the recurrence of such incidents.
6. Analysis and Action
The primary purpose of incident analysis is to understand how and why the incident occurred, and to identify ways of preventing a recurrence. The analysis should take into account information gathered during the investigation and classification phases. Actions and recommendations are developed to prevent recurrence of the incident.
A timeframe for the implementation of recommendations from incident investigations is documented in the incident register with action taken within 60 working days of incident notification.
The Directors review any recommendation and if accepted, records the acceptance of recommendations and comments once the recommendations have been accepted.
Postural Innovations will analyse their own incident data through the monitoring of trend and aggregate reports.
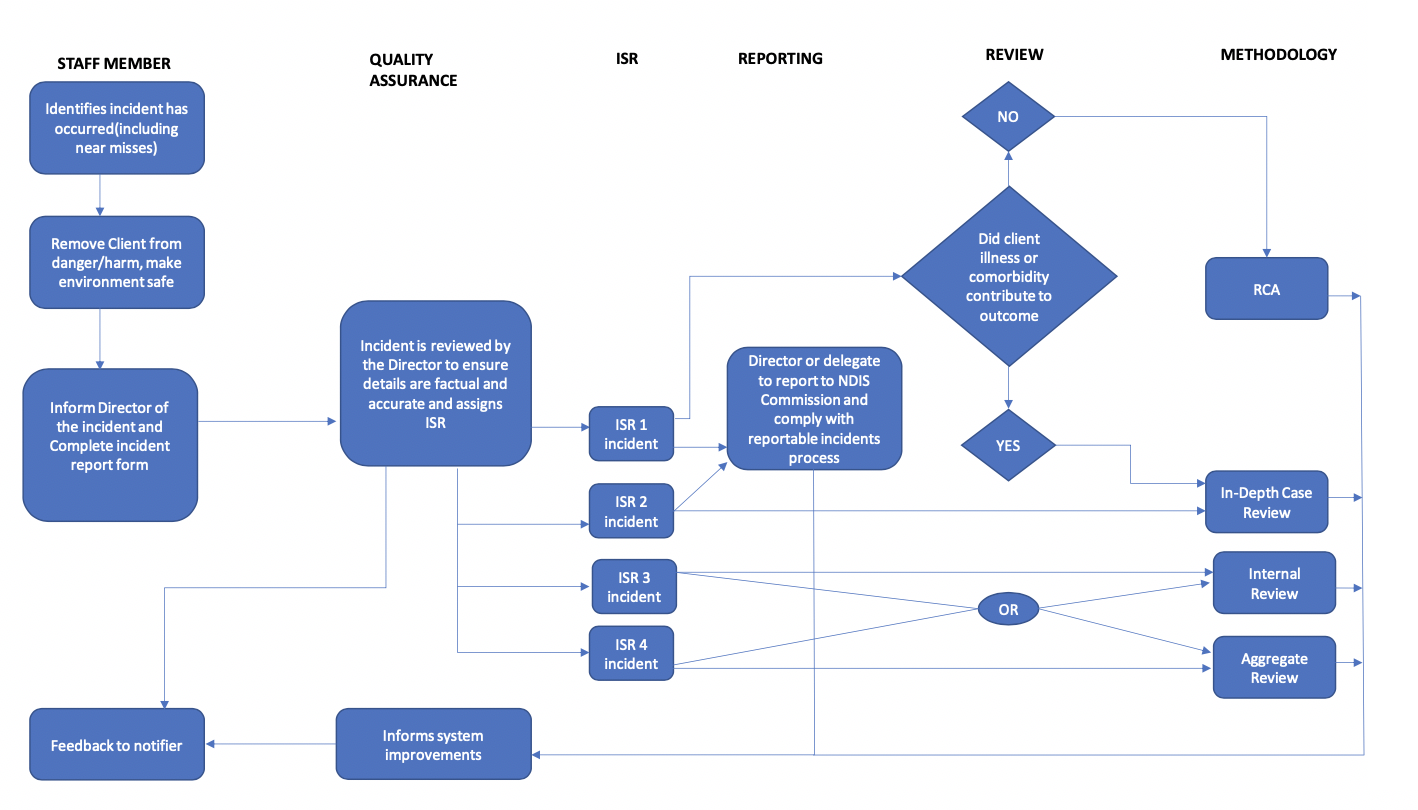
Postural Innovations Steps in Incident Management
7. Feedback
Feedback is an important component of a successful incident management program.
Feedback to Clients and Support Persons – Open Disclosure
Information about ISR 1 and 2 clinical incidents should be offered to the Client or their support person. This feedback process reflects principles of the open disclosure process.
The information provided to a person can be based on a variety of sources, but above all should be factual and presented in a manner which is understood by the recipient audience. The Summary Report from an RCA is one of the sources which may be used in providing feedback on a clinical ISR 1 incident.
The principles of open disclosure should be observed throughout the feedback process, refer to Clinical Risk Management for additional information on this process.
Feedback to Staff
It is well-documented the success of incident management systems, regardless of their level of sophistication, is dependent on feedback to staff on the results and outcomes of investigations in a timely manner.
It is imperative staff involved in an incident be informed of the recommendations arising from any investigation. The summary RCA report provides the basis for feedback on a clinical ISR 1 incident. The findings of these and other incidents will be given to the relevant staff and care team.
Regular reports on trended aggregate incident data and outcomes of clinical case reviews and other forms of investigation should be provided to staff.
Feedback should also include the changes made and improvements achieved as a result of these amendments to practice.
Record Keeping
Postural Innovations will keep hard copies of any Postural Innovations Incident and Hazard Report Form completed and filed in a secure folder. Electronic copies of the Postural Innovations Incident and Hazard Report Form are also filed and kept securely on the Postural Innovations SharePoint as well as entered into the Postural Innovations Incident Reporting Log.
Incident and near-misses are recorded in the Incident Reporting Log on SharePoint and hazards are recorded in the Hazard Identification Register on SharePoint.
Any correspondence between Postural Innovations and the Client or support person is recorded in SharePoint.
Definition – Degree of Impact
Where harm includes disease, injury, suffering, disability and death:
disease – a physiological or psychological dysfunction;
injury – damage to tissues caused by an agent or circumstance;
suffering – experiencing anything subjectively unpleasant. This may include pain, malaise, nausea, vomiting, loss (any negative consequence, including financial) depression, agitation, alarm, fear or grief;
disability – any type of impairment of body structure or function, activity limitation and/or restriction of participation in society, associated with a past or present harm.
| Degree of Impact | Description |
|---|---|
| No harm – did not reach the subject | There was no harm to the subject, that is, the incident did not reach the subject. |
| No harm – did reach the subject | The incident reached the subject, but there was no harm caused. |
| No harm – significantly inconvenienced | The subject was significantly inconvenienced in relation to time, travel, wages, lifestyle and family impact as a result of the issue and/or incident. |
| Harm – but no loss or reduction in functioning | The subject experienced harm but did not have a loss or reduction in functioning as a result of the incident. |
| Harm – temporary reduction in functioning | One or more systems or components of the subject’s body are able to operate, fulfilling their purpose or role, but not to the level they could prior to the incident. The subject is likely to recover from this reduction in the short-medium term. |
| Harm – temporary loss in functioning | One or more systems or components of the subject’s body are no longer able to operate normally, fulfilling their purpose or role. The subject is likely to recover from this loss within the short-medium term. |
| Harm – permanent reduction in functioning | One or more systems or components of the subject’s body are able to operate, fulfilling their purpose or role, but not to the level they could prior to the incident. The subject is not likely to recover from this reduction. |
| Harm – permanent loss in functioning | One or more systems or components of the subject’s body are no longer able to operate normally, fulfil their purpose or role. The subject is not likely to recover from this loss. |
| Harm – death | The subject died unexpectedly at the time of, or following, the incident (e.g. major car accident while transporting a Client for community access shifts; drowning during hydrotherapy; fatal fall during therapy session; natural causes such as epileptic seizure, heart attack, stroke, storm asthma; medication overdose; first aid events, etc. |
| Unknown | The degree of harm caused to the subject, due to the incident, is not known at this time. |
Definition – Level of Care
| Level of Care | Description |
|---|---|
| No significant change | The subject did not require any significant extra care or higher care as a result of the incident. |
| Current setting – increased observation, monitoring | The subject required increased observation, monitoring. The subject was not transferred elsewhere to a higher level of care. |
| External transfer – non inpatient | The subject was transferred externally to a hospital for care but was not admitted. |
| External transfer – inpatient admission | The subject was transferred externally to a hospital for a higher level of care and was admitted. |
| Not applicable | The level of care is set to ‘not applicable’ when the degree of impact was ‘death’. |
| Unknown | The change in level of care required by the subject, due to the incident, is not known at this time. |
Definition – Treatment Required
| Treatment Required | Description |
|---|---|
| No treatment | Following a clinical review, intervention was deemed not required. |
| Minor treatment including first aid | The subject required a simple or minor intervention as a result of the incident (e.g. wound dressings, medications such as paracetamol, etc.) |
| Advanced treatment | The subject required significant medical, diagnostic or surgical intervention as a result of the incident which required an ambulance to transfer the patient to a hospital (e.g. MRI, CT, medications such as adrenaline, etc.) |
| Not applicable | The treatment required is set to ‘not applicable’ when the degree of impact was ‘death’. |
Examples of ISR
ISR 1: Severe/Death
Severe injury to a person with a disability or death of a person with a disability – such as a fatal car accident while transporting a Client for community access shifts; drowning during hydrotherapy; fatal fall during a therapy session; natural causes such as epileptic seizure, heart attack, stroke, storm asthma; medication overdose; first aid events; etc.
Severe injury to clients and/or carers requiring medical treatment/hospitalisation.
Any incident involving the police, fire or ambulance services.
Serious injury to employees requiring medical treatment/hospitalisation.
Events which may be of significant interest to the media.
ISR 2: Major
The abuse or neglect of a person with disability; the unlawful sexual or physical contact with, or assault of, a person with disability; sexual misconduct committed against, or in the presence of, a person with disability, including grooming of the person for sexual activity.
Injuries to Employees requiring First Aid.
Injuries to Clients and/or carers requiring First Aid.
Significant property damage.
ISR 3: Moderate
Non severe injury to a person with a disability but harm is done
Aggressive and verbal abuse to employee.
ISR 4: Minor – Near miss / No harm
Minor injury to a Client and/or their carer – First Aid not required.
Minor injury to an Employee – First Aid not required.
Minor property damage.